It is curious to note how, in emergency situations, proposals appear that promise quick, safe and “natural” solutions. This is nothing new; we have already seen things like this in dengue epidemics, COVID-19 and cancer treatment. Even more worryingly, this has also found its way into obstetric emergencies, such as the “study” entitled “Use of Acupuncture in Cases of Hypertensive Emergencies during Pregnancy”.
Based on parts of a final paper for a postgraduate course in Acupuncture at CETN (Center for Studies of Natural Therapies), the supposed study illustrates the problem well: it is an experimental proposal that does not produce useful results, can delay conventional treatment and put the lives of pregnant women at risk.
The “study” in question reports cases of pregnant women with hypertension – supposedly classified as “hypertensive emergencies” – who underwent auricular acupuncture and bleeding from the apex of the ear, with the aim of reducing blood pressure. Although the text mentions the possibility of drug treatment after an initial “stabilization”, it is clear that alternative interventions were prioritised as the first treatment, instead of effective and urgent management of the hypertensive condition. This is alarming; an obstetric emergency cannot be held hostage by therapies without demonstrated efficacy and safety.
As is usual in “studies” of this type, the absence of a rigorous methodology is clearly evident: there is no control group (or, if there is, it is not adequately presented), the exact number of patients analysed is unknown (the number of participants in each subgroup is not even mentioned), there is no information on whether there was randomisation (probably non-existent, given the lack of a control group), nor is there any description of any type of reliable diagnostic criterion for classifying blood pressure as a “hypertensive emergency”. On the contrary, the cutoff point for considering inclusion in the study was a pressure above 120×80 mmHg; a value that, let’s face it, does not constitute an urgent or emergency condition according to any cardiology or obstetrics guidelines.
It is plausible that most of these patients, therefore, were not even in a condition of imminent risk, which calls into question any supposed effectiveness of the practice.
Pre-eclampsia
Pre-eclampsia is generally characterised by high blood pressure (systolic pressure above 140 and/or diastolic pressure above 90 mmHg) after the 20th week of pregnancy, associated with high levels of protein in the urine and/or target organ dysfunction. We are not talking about a condition caused by “stress” or something emotional, but rather a complex problem, based on genetic, immunological and vascular factors. Patients with preeclampsia may progress to eclampsia, a condition that involves seizures and risk of coma, or develop potentially fatal complications, such as HELLP syndrome (Haemolysis, Elevated Liver Enzymes and Low Platelet Count), kidney failure, premature placental abruption, premature birth and even maternal and/or foetal death.
This “alternative protocol” draws attention precisely because it is indicative of a larger problem: the spread of pseudoscientific practices in healthcare. It perfectly exemplifies the creation of a seductive narrative to justify unfounded treatments. The original text evokes concepts from Traditional Chinese Medicine to explain pre-eclampsia, such as “wind rising from the liver”, “Yin deficiency” or “damp-heat”, without, at any point, providing evidence for this.
By trying to “fit” a very serious obstetric condition, such as pre-eclampsia, into merely traditional standards that have not been validated in the medical-scientific sphere, they attempt to legitimise dangerous practices that can delay or replace treatments that would have a real impact on reducing complications and maternal and foetal mortality.
The rush that saves lives
In obstetric emergencies, every minute counts. Pre-eclampsia can worsen rapidly, leading to seizures, pulmonary oedema, and other serious complications. If the patient is led to believe that “natural” measures must come first, she risks losing valuable time before receiving proven effective medication. The momentary feeling of “wellbeing,” without monitoring and without adequate monitoring of vital signs, can mask progression to lethal stages.
Just look at the main guidelines of major entities – such as the American College of Obstetrics and Gynaecology (ACOG), the International Society for the Study of Hypertension in Pregnancy (ISSHP), the Brazilian Network for the Study of Hypertension in Pregnancy (RBEHG) or even the World Health Organization (WHO) – to see that none of them recommend an “integrative” treatment as an initial approach to the crisis, much less for hypertensive emergency.
On the contrary, all of them indicate immediate clinical intervention, not only with the use of antihypertensives that are safe for pregnancy (such as nifedipine, hydralazine and, where available, labetalol), but also with the use of magnesium sulphate, which is essential for the prevention of seizures, careful evaluation of foetal well-being, hospitalisation, intensive monitoring in the most severe cases and, depending on the severity and gestational age, termination of pregnancy.
It is understandable that pregnant women may be afraid of medications, especially if they are uncertain about side effects or risks to the foetus. Unfortunately, this uncertainty leaves room for promises of “harmless” or “chemical-free” techniques.
The result is dangerous confusion, since what is at stake is the health of both mother and baby. When it comes to pre-eclampsia, supposed temporary relief does not guarantee that the disease will not continue to advance silently.
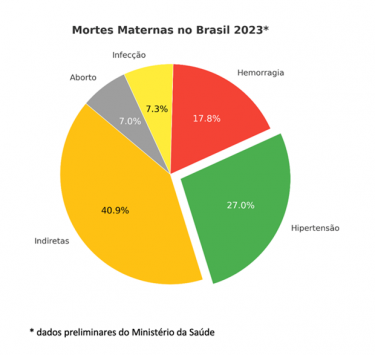
Added to this is our harsh reality: hypertension is the leading cause of direct maternal death in Brazil (and the leading cause as an isolated cause). We need more efficient prenatal care and quick responses when signs of pre-eclampsia appear, not dubious protocols that further delay correct referral.
Pseudoscientific bingo
This study serves as a perfect example of pseudoscientific logic, featuring elements that are common to this type of biased study:
- Lack of explicit inclusion criteria and use of outdated nomenclature: women with blood pressure above 120×80 mmHg were labeled as having a “hypertensive emergency”. This is a gross mistake, as it does not comply with international standards. Furthermore, the article uses nomenclature that is no longer in use, such as DHEG (hypertensive disease specific to pregnancy).
- Hasty conclusions: based on specific observations, the author concludes that “in 61.5% of cases, acupuncture was successful in reducing blood pressure levels”. Success based on what parameters? How long does this supposed effect last?
- Absence of a control group: no comparison is made with pregnant women who simply rested and then had their blood pressure measured (which would not be indicated in an emergency, but is recommended in hypertensive crises, after 15 minutes, since with rest, in the latter, the blood pressure can actually drop); or pregnant women who received standard treatment with appropriate medications; or even pregnant women who received another harmless intervention (placebo). Without control, there can be no talk of efficacy. And when there is no evidence of efficacy, there is no therapeutic effectiveness, as we have already discussed.
- Confusion between correlation and causation: Given the lack of reliable methodology, the study cannot prove that it was acupuncture that reduced blood pressure – or even that it was dangerously high at the beginning of the study.
- Omission of critical data: no report of loss to follow-up (if patients returned to the emergency room with worsening of their condition), no mention of relevant maternal or neonatal outcomes (e.g. maternal mortality, neonatal mortality, incidence of eclampsia, neurological damage, etc.).
- Vague, grandiose (and dangerous) claims: The final message that auriculotherapy “can be used to reduce blood pressure levels in pregnant women seeking emergency services” states much more than the data presented allows us to conclude. And worse, readers of the article may understand that it is acceptable to refuse or postpone obstetric management recommended by medical guidelines, believing in a false solution.
- The “complementary” discourse: Advocates of alternative therapies often argue that they do not want to replace evidence-based practices, but rather complement them. In an ideal world, this justification might even sound reasonable. However, in practice, we see that such interventions are often presented as sufficient or as “first line” (as, in fact, this study suggests). Furthermore, time and money are both scarce resources. In this way, the “complementary” ends up becoming a trap that takes the focus away from what really needs to be done – and, in this case, done quickly.
- “Emotional” causes for multifactorial organic issues: many “alternative interventions” are based on the mistaken notion that high blood pressure (especially during pregnancy) is the result exclusively of stress or emotional changes. We do not deny that psychological factors can momentarily affect blood pressure, but the pathophysiology of preeclampsia cannot be explained by “excessive nervousness” or anxiety. Reducing the complexity of this issue to a purely “psychoemotional” issue creates the dangerous feeling that simply relaxing (with lavender, teas, foot baths or auriculotherapy) is enough to control blood pressure. Patients with blood pressure lability (blood pressure that “rises with stress”) or with white coat hypertension (blood pressure that only rises during a medical appointment) have a higher risk of developing pre-eclampsia. This in itself is already a warning sign, requiring medical referral.
Systemic problem
Unfortunately, this study is not just an isolated daydream; it reveals what often happens when people in vulnerable situations (such as pregnant women) encounter, in the health system or on social networks, professionals who offer “quick and natural solutions” to serious problems. These are solutions based on beliefs without scientific basis and which can delay effective care.
This is not about demonising any practice that is not strictly pharmacological. The problem here is the use of unvalidated therapies as substitutes or barriers to conventional treatment, especially when the clock is ticking. The idea that “it doesn’t hurt to try” ignores the risk of delaying effective interventions.
There is also a social dimension. A poorly founded study, but with the guise of “academic research,” may be disseminated in lectures, social networks, or less discerning media outlets. Many people firmly believe that everything they discover through Google searches and online pages is true. Patients who read about the subject on the internet may ask: “Why not try acupuncture first, since an article said it works and is less invasive?” Not to mention the cases in which authorities and professional associations end up legitimising such practices simply because of their popularity.

The role of professionals who fight for a more scientific medicine is to monitor, report and inform the population about the risks involved in practices like this. There is no room, in emergency situations, for “experimental therapies” that do not meet the basic criteria of plausibility and ethical criteria of clinical research.
Final considerations
By proposing (and promoting) auricular acupuncture as a priority intervention in “hypertensive emergencies” during pregnancy, the “study” risks confusing professionals and patients, since the mere appearance of “academic research” may give a false impression of legitimacy. Although the initiative presents itself as “experimental,” it does not meet the scientific criteria required for this. The lack of an adequate methodological design, the absence of a control group, and the incorrect definition of the inclusion criteria seriously compromise the validity of the results presented.
Even more alarming is the fact that, under the guise of an experimental protocol, pregnant women were subjected to an intervention that delayed the administration of proven-effective conventional treatments, which constitutes a flagrant ethical violation. We were unable to find the aforementioned study published in any national or international journal, which in fact seems impossible to us, given so many serious problems and biases. However, we assume that it was approved by a Research Ethics Committee (REC), which, if proven, is unacceptable. How can a research project to treat hypertensive emergencies with auriculotherapy be authorised? How can a study with so many methodological flaws be allowed?
The real line in healthcare is not between “conventional” and “alternative” medicine, but between what is evidence-based and what is not. In emergencies, we cannot forgo what really works. If there is one lesson from this episode, it is the warning it provides: maternal health is not a place of illusion. When dealing with pre-eclampsia and eclampsia, every minute of delay in providing appropriate care can cost a life – or two.



